Please click the frequently asked questions below for further information and IPC precautions required:
What is C.diff?
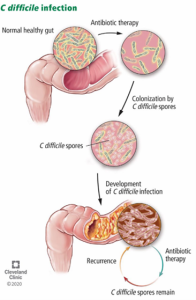
Clostridioides difficile infection (C. difficile) , also known as Clostridium difficile, is a major cause of infectious diarrhoea due to the spore-forming bacterium, Clostridioides difficile. It is predominantly healthcare associated and accounts for about 20% of cases of antibiotic-associated diarrhoea.
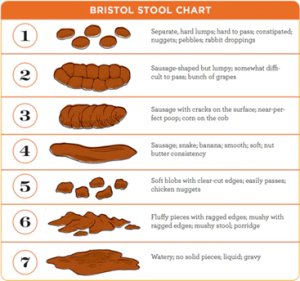
Disease is mediated by the production of toxins, and symptoms include watery diarrhoea, fever, nausea, and abdominal pain, which may lead to serious complications including pseudomembranous colitis, toxic megacolon, and death.
Those at most risk of developing C. difficile include elderly people and immunocompromised patients. A small proportion of healthy adults may carry C. difficile as part of the normal gut flora.

Where are the main symptoms of C.diff?
- The main symptom is explosive diarrhoea which has a particularly unpleasant smell.
- Other symptoms include stomach cramps, fever, nausea and loss of appetite.
- Most people become only mildly ill and then recover fully.
- The vast majority of patients make a straightforward recovery.
- Some patients may become seriously ill and develop inflammation of the bowel (colitis). If the colitis is severe it can be life-threatening
Symptoms may last from a few days to several weeks.
Why is this information important?
If NIAS staff are aware that the patient an active infection of C.diff or patients experiencing diarrhoea, this should be communicated to the Control Room (Emergency or Non-emergency as appropriate) and the staff in the receiving unit when transferring the patient to ensure effective patient care and management.
NIAS staff should ensure that all patients who are symptomatic of Infective diarrhoea should be risk assessed for a C.diff infection.
How is it spread?
C.diff can be ingested and spread between patients either through contact with a patient known C.diff infection / have current C.diff carriage or by touching the environment that has been occupied by a patient with C.diff e.g. patient equipment, stretchers, hand rails, straps etc.
It can also be spread through staff’s hands if staff do not adhere to the 5 moments of Hand Hygiene (HH) using the 7 step technique. It is also essential that staff use PPE appropriately ensuring that gloves are used and changed appropriately with HH. This will help protect both staff and patients from transmission of C.diff.
IPC Precautions
- Contact Precautions should be used
- Hand Hygiene should be completed as per the 5 moments in line with usual practice. HH should be completed with Soap and Water.
- Eye protection should always be risk assessed and used with any patient where there is a risk of splashes including spitting and productive coughing.
- Gloves and Aprons should be worn.
- The patient should be transported via ambulance (eg. PCS) with no other patients present where possible. Individual cases can be discussed with the IPC team and a risk assessment can be made.
- Laundry should be treated as contaminated, placed into an alginate bag and placed into a red laundry bag.
What cleaning is required?
All equipment and the ambulance should have an in-between patient clean with a hypochlorite solution paying particular attention to all staff and patient touch points. If the patient is a known carrier with no active diarrhoea, then a standard in-between patient clean can be completed.
Do staff need any prophylaxis or follow up?
No staff follow up required.
