Please click the frequently asked questions below for further information and IPC precautions required:
What is Transmissible spongiform encephalopathies (TSEs)?
TSEs or prion diseases, are a group of rare and invariably fatal neurodegenerative disorders.
Three types of TSE can affect humans:
- idiopathic TSEs (e.g. sporadic Creutzfeldt-Jakob disease [CJD])
- familial TSEs
- acquired TSEs (e.g. iatrogenic CJD)
How does it spread?
Latrogenic transmission from cases of sporadic CJD can occur in association with specific medical interventions, including:
- receipt of hormones derived from human pituitary glands (i.e. growth hormone and gonadotrophin)
- organ or tissue transplants (i.e. dura mater grafts and corneal transplantation)
- neurosurgical procedures using contaminated instruments.
With the exception of neurosurgical procedures, these interventions are no longer performed in the UK.
Abnormal prion proteins can remain infective on instruments after steam sterilisation and are highly resistant to both chemical disinfectants and radiation. Iatrogenic transmission from cases of vCJD can occur via blood transfusion or receipt of blood products (e.g. clotting factors).
What are the symptoms of TSEs?
Variant CJD (vCJD) is an acquired TSE caused by transmission of the agent responsible for bovine spongiform encephalopathy (BSE) in cattle. Whereas sporadic CJD is most common in people over 50 and accounts for 85% of CJD cases, vCJD has an age of onset in the late 20s.
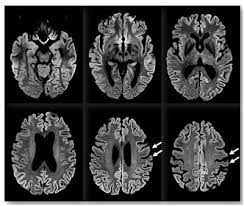
Sporadic CJD presents as rapidly progressive dementia with a range of neurological signs and symptoms, including ataxia, myoclonus, visual disturbances and movement disorders. In vCJD, this presentation is often preceded by psychiatric symptoms, such as anxiety and depression.
People with vCJD tend to live for an average of 14 months after symptom onset, while survival for sporadic CJD is frequently only a few months.
Why is this important?
If NIAS staff are aware that the patient has a suspected or confirmed case this should be communicated to the Control Room (Emergency or Non-emergency as appropriate) and the staff in the receiving unit when transferring the patient to ensure effective patient care and management.
IPC Precautions
- Standard Precautions should be used.
- Hand Hygiene should be completed as per the 5 moments in line with usual practice.
- Eye protection should be risk assessed for any concern regarding a splash risk.
- Gloves and Aprons should be risk assessed
- Laundry should be treated asper usual policy.
What cleaning is required?
All equipment and the ambulance should have an in-between patient clean paying particular attention to frequent touch points.
Do staff need prophylaxis or follow up?
No staff follow up required.
