Please click the frequently asked questions below for further information and IPC precautions required:
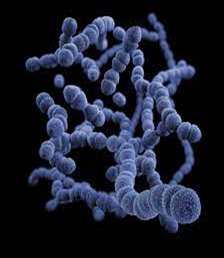
What is Streptococcus pneumoniae?
Streptococcus pneumoniae is a member of the Streptococcus family and is the bacterium responsible for causing pneumococcal infections. It is a normal part of the upper respiratory tract flora, however can become pathogenic with 90 different pneumococcal types (serotypes) that can cause diseases in humans.
There are two pneumococcal vaccines that can help to protect against pneumococcal disease; one is part of the routine childhood immunisation schedule, whilst the other is for those aged 65 and over or for those under 65 with certain underlying co-morbidities.
How does it spread?
It is a Contact Spread organism. Transmission is possible from contact with colonised environmental sources or the skin of colonised individuals.
What are the symptoms of Streptococcus pneumoniae?
Pneumococcal infections are classified as invasive or non-invasive depending on the site affected and include; bronchitis, otitis media, acute sinusitis and conjunctivitis amongst others, and are also one of the leading causes of pneumonia. The elderly, young children (particularly neonates), and people who are immunocompromised are the most susceptible.
Invasive Pneumococcal Diseases (IPD) are pneumococcal infections of sterile sites, such as blood, cerebrospinal fluid (CSF) caused by S. pneumoniae. They are a major cause of morbidity and mortality, especially in the very young, elderly and people who are immunocompromised.
Pneumococcal meningitis is a type of IPD and one of the most frequently reported causes of meningitis. Signs and symptoms include headache, fever, nausea and vomiting, stiffness of the neck and photophobia.
Why is this important?
If NIAS staff are aware that the patient has a suspected or confirmed Streptococcus pneumoniae, this should be communicated to EAC / NEAC and the receiving unit when transferring the patient to ensure effective patient care and management. This is particularly essential if the patient is immunosuppressed or is being admitted to NICU or other augmented care areas.
IPC Precautions
- Standard Precautions should be used.
- Contact Precautions may be required with high risk patients such as those who are immunosuppressed or Neonates. This can be discussed with the IPC team.
- Hand Hygiene should be completed as per the 5 moments in line with usual practice.
- Eye protection should be risk assessed for any concern regarding a splash risk.
- Gloves and Aprons should be risk assessed and worn if contact with the patient’s blood or bodily fluids.
- Laundry should be treated as per standard policy.
What cleaning is required?
All equipment and the ambulance should have an in-between patient clean, paying particular attention to touch points.
Do staff need prophylaxis or follow up?
No follow up required.
