Please click the frequently asked questions below for further information and IPC precautions required:
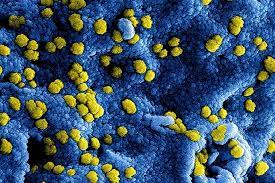
What is MERS?
This is a novel coronavirus that emerged in the Middle East and is classed as a high consequence infectious disease (HCID). It causes severe viral respiratory disease.
How does it spread?
MERS-CoV, like other coronaviruses, likely spreads from an infected person’s respiratory secretions, such as through coughing. However, we don’t fully understand the precise ways that it spreads.
MERS-CoV has spread from ill people to others through close contact, such as caring for or living with an infected person. Infected people have spread MERS-CoV to others in healthcare settings, such as hospitals.
Those at risk of contracting MERS-CoV include travellers to the Arabian Peninsula (or those in close contact with travellers to this region). The camel is a host species for the virus and those in contact with camels or camel products may also be at risk of contracting the disease.
What are the symptoms of MERS?
Symptoms include fever and cough that commonly progresses to a severe pneumonia, sometimes requiring mechanical ventilation. Pneumonia is more likely in immunocompromised individuals, people with cardiopulmonary illnesses, as well as the elderly and young children. In some cases, a diarrhoeal illness has been the first symptom to appear.
Why is this important?
If NIAS staff are aware that the patient has a suspected or confirmed MERS-CoV, this should be communicated to EAC / NEAC and the IPC Team as soon as possible. Where possible the HART team will convey patients who are a high level of suspicion or confirmed case of MERS-CoV.
All MERS-CoV cases are notifiable to the Public Health Agency (PHA).
IPC Precautions
- This should be treated as a HCID.
- The HART team should be involved in risk assessment and transfer of all suspected and confirmed cases.
- As this is a HCID there are specific guidelines surrounding the use of PPE. Guidance should be sought for the appropriate method of donning and doffing of PPE.
- An FFP3 mask that you are fit tested for should be used.
- Ensure use of a buddy system for donning and doffing PPE.
The NIAS guidance for VHF should be used and the IPC team contacted immediately for further advice.
What cleaning is required?
- All equipment and the ambulance should have a deep clean with a hypochlorite solution with a strength of 10,000 PPM (Same dilution as blood and body fluids).
- Appropriate PPE should be worn when decontaminating the vehicle and the equipment.
- Any single use equipment should be disposed of.
- Waste should be treated as Category 4 waste and disposed of in line with the trust waste.
Do staff need prophylaxis or follow up?
A list of staff will be recorded of all staff who have had interaction with the suspected/confirmed case.
All staff in contact with a case of MERS will be individually risk assessed by the multi-agency team.
