Please click the frequently asked questions below for further information and IPC precautions required:
-
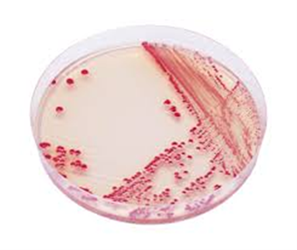
What is Acinetobacter baumannii?
Acinetobacter baumannii is a gram-negative bacterium that is found in the environment including
drinking water, soil and sewage. It can also be found on the skin of some healthy individuals. A.baumannii infections in the community are very rare and almost exclusively occur in the hospital setting. It is an opportunistic pathogen affecting those with underlying health problems and infection is often associated with invasive or indwelling medical devices.
Infections can be very difficult to treat as A.baumannii is intrinsically resistant to many antimicrobial agents and can acquire resistance easily. This includes increasing resistance to the carbapenem class of antibiotics which are often the last resort for treatment.

-
How does it spread?
It is a Contact Spread organism.
Transmission is possible from contact with colonised environmental sources or the skin of colonised individuals.
-
What are the symptoms of Burkholderia?
A.baumannii can cause pneumonia, bloodstream infections, meningitis, urinary tract infections an surgical site infections including necrotising fasciitis. Symptoms will depend on the area of the body affected.
At risk groups include patients who are immunocompromised, have chronic lung disease, diabetes, or burn injuries.
-
Why is this important?
If NIAS staff are aware that the patient has a suspected or confirmed case this should be communicated to the Control Room (Emergency or Non-emergency as appropriate) and the staff in the receiving unit when transferring the patient to ensure effective patient care and management.
-
IPC Precautions
- Standard Precautions should be used.
- Contact Precautions may be required with high risk patients such as those with Cystic Fibrosis and Neonates.
- Hand Hygiene should be completed as per the 5 moments in line with usual practice.
- Eye protection should be risk assessed for any concern regarding a splash risk.
- Gloves and Aprons should be risk assessed and worn if contact with the patient’s blood or bodily fluids.
- Laundry should be treated as contaminated, placed into an alginate bag and placed into a red laundry bag.
-
What cleaning is required?
All equipment and the ambulance should have an in-between patient clean, paying particular attention to touch points.
-
Do staff need prophylaxis or follow up?
No staff follow up required.
The IPC team can be contacted for further advice. The team will be able to help staff risk assess the patient and precautions required and to provide support where required.




