Please click the frequently asked questions below for further information and IPC precautions required:
-
What is Campylobacter?
Campylobacter is a gram-negative, microaerophilic genus of bacteria of the family Campylobacteriacae. There are more than 20 species of Campylobacter, not all of which cause human illness. Approximately 90% of human Campylobacter illness is caused by one species, Campylobacter jejuni.

-
Why is this information important?
If NIAS staff are aware that the patient is potentially symptomatic or a confirmed case of Campylobacter then this should be communicated to EAC and ED staff when transferring the patient to ensure effective patient care and management.
-
How is it spread?
Most cases of Campylobacter infection occur after someone eats raw or undercooked poultry or another food that has been contaminated by raw or undercooked poultry.
Outbreaks of Campylobacter infection are infrequently reported relative to the number of illnesses. Outbreaks have been associated with unpasteurized dairy products, contaminated water, poultry, and produce.
People also can get infected from contact with dog or cat feces.
Person-to-person spread of Campylobacter is uncommon but can be transmitted if direct contact with contaminated vomit or feaces.
Patients should continue to be considered infectious while symptomatic.
-
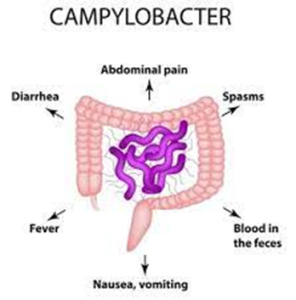
What are the symptoms of Campylobacter?
Symptoms usually includes:
- Diarrhoea (often bloody)
- Fever
- Stomach cramps
- Nausea and vomiting may accompany the diarrhoea
These symptoms usually start 2 to 5 days after the person ingests Campylobacter and last about one week.
Sometimes Campylobacter infections cause complications, such as irritable bowel syndrome, temporary paralysis, and arthritis.
In people with weakened immune systems, such as those with a blood disorder, with AIDS, or receiving chemotherapy, Campylobacter occasionally spreads to the bloodstream and causes a life-threatening infection.
-
IPC Precautions
- Hand Hygiene should be completed as per the 5 moments in line with usual practice with Soap and Water
- Eye protection should be risk assessed and worn if any risk of splashes.
- Gloves and Aprons should be worn.
- The patient should be transported via ambulance with no other patients present.
- All equipment and the ambulance should have a deep clean paying particular attention to touch points.
- Laundry should be treated as contaminated, placed into an alginate bag and placed into a red laundry bag.
-
What Cleaning is required?
All equipment and the ambulance should have an in-between patient clean paying particular attention to touch points.
-
Do staff need any prophylaxis or follow up?
If staff have been exposed to a confirmed or suspected case of Campylobacter they should remain vigilant for any symptoms but there is no active follow up required.
If staff become symptomatic they should remain off work until 48 hours asymptomatic (72 hours if food handling).
The IPC team can be contacted for further advice. The team will be able to help staff risk assess the patient and precautions required and to provide support where required.




