Please click the frequently asked questions below for further information and IPC precautions required:
-
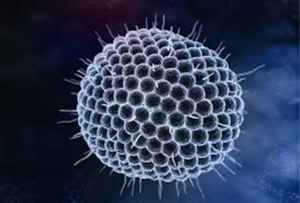
What is Chickenpox?
Chickenpox is a highly contagious disease caused by the varicella-zoster virus (VZV). It can cause an itchy, blister-like rash among other symptoms. The rash first appears on the chest, back, and face, and then spreads over the entire body.
Chickenpox can be serious, especially during pregnancy, in babies, adolescents, adults, and people with weakened immune systems (lowered ability to fight germs and sickness).
-
Why is this information important?
If NIAS staff are aware that the patient has a suspected or confirmed case this should be communicated to the Control Room (Emergency or Non-emergency as appropriate) and the staff in the receiving unit when transferring the patient to ensure effective patient care and management.
-
How is it spread?
See Shingles section for further information.
-
What are the symptoms of Chickenpox?
Anyone who has not had chickenpox or gotten the chickenpox vaccine can get the disease. Chickenpox illness usually lasts about 4 to 7 days.
The classic symptom of chickenpox is a rash that turns into itchy, fluid-filled blisters that eventually turn into scabs. The rash may first show up on the chest, back, and face, and then spread over the entire body, including inside the mouth, eyelids, or genital area. It usually takes about one week for all of the blisters to become scabs.
Other typical symptoms that may begin to appear one to two days before rash include:
- fever
- tiredness
- loss of appetite
- headache
-
IPC Precautions
- Airborne Precautions should be worn by all staff who are not known to be immune to chickenpox
- Hand Hygiene should be completed as per the 5 moments in line with usual practice.
- Eye protection should be worn by staff who have no known immunity to chickenpox.
- FFP3 Mask should be worn by staff who have no known immunity to chickenpox.
- Gloves and Aprons should be worn.
- The patient should be transported via ambulance with no other patients present.
- Ideally should be care for by staff with a known immunity and those not in a high risk category including immunosuppression and pregnancy.
- Laundry should be treated as contaminated, placed into an alginate bag and placed into a red laundry bag.
-
What Cleaning is required?
All equipment and the ambulance should have an in-between patient clean paying particular attention to touch points.
-
Do staff need any prophylaxis or follow up?
If staff have been exposed to a confirmed or suspected case of chickenpox the Line Manager and the IPC team should be contacted to ensure a risk assessment is completed.
If required the staff member will be referred to Occupational Health.
Significant Exposure includes Non-immune individuals who have had:
- Non-close contact in the same room as a person with chickenpox (e.g. in a house, classroom, hospital bay/ dayroom) for 15 minutes or more
- Close contact (more than 5 minutes) with a person with chickenpox
- Contact with disseminated shingles and exposed lesions e.g. ophthalmic shingles
- Contact with immunosuppressed patients with shingles
Staff who have a known immunity:
- Do not need post exposure prophylaxis
- Do not need work restrictions
- Links to Guidance:




