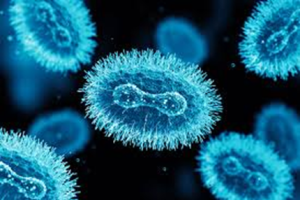
Mpox (previously known as monkeypox) is a rare disease caused by infection with the mpox virus. Mpox virus is part of the same family of viruses as variola virus, the virus that causes smallpox. Mpox symptoms are similar to smallpox symptoms, but milder, and mpox is rarely fatal. Mpox is not related to chickenpox.
Mpox was first discovered in 1958 when outbreaks of pox like disease occurred in monkeys kept for research. The first human case was recorded in 1970 on the Democratic Republic of Congo (DRC). Since then it has been occurred in several African countries, before 2022 most cases were reported in DRC and Nigeria.
There are 2 main genetic groups of Mpox known as clades. In 2022 cases of human Mpox were reported in multiple counties including the UK and Ireland. This is was associated with sexual activity and was caused by Mpox Clade II. Clade II is no longer considered a High Consequence Infectious Disease (HCID) in the UK.