Please click the frequently asked questions below for further information and IPC precautions required:
-
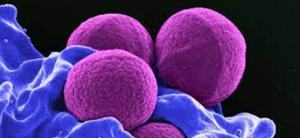
What is MRSA?
MRSA is meticillin (previously known as methicillin) resistant Staphylococcus aureus.
Staphylococcus aureus is a common germ that can live harmlessly on the skin and/or in the nose of about 1 in 3 people. MRSA is a type of Staphylococcus aureus that has become resistant to a number of different antibiotics. However, effective treatment is available.
Most people who are carrying MRSA on their bodies or in their nose don’t suffer any ill effects. However, if someone has MRSA infection, they will be unwell and have symptoms of infection, such as pain, high temperature, soreness/swelling at site of infection.
-
Where are the most common places to detect MRSA?
MRSA is commonly found in the nose, back of the throat, armpits, skin folds of the groin and in wounds. The only way to know if you have MRSA is by sending a swab or a sample, such as urine, to the hospital laboratory for testing.

-
Why is this information important?
If NIAS staff are aware that the patient has a suspected or confirmed case this should be communicated to the Control Room (Emergency or Non-emergency as appropriate) and the staff in the receiving unit when transferring the patient to ensure effective patient care and management.
-
How is it spread?
MRSA can spread between patients either through contact with a patient known to have MRSA or by touching the environment that has been occupied by a patient with MRSA e.g. patient equipment, stretchers, hand rails, straps etc.
It can also be spread through staff’s hands if staff do not adhere to the 5 moments of Hand Hygiene (HH) using the 7 step technique. It is also essential that staff use PPE appropriately ensuring that gloves are used and changed appropriately with HH. This will help protect both staff and patients from transmission of MRSA.

-
IPC Precautions
- Contact precautions should be used
- Hand Hygiene should be completed as per the 5 moments in line with usual practice.
- Eye protection should always be risk assessed and used with any patient where there is a risk of splashes including spitting and productive coughing.
- Gloves and Aprons should be worn.
- The patient should ideally be transported via ambulance (eg. PCS) with no other patients present where possible. Individual cases can be discussed with the IPC team and a risk assessment can be made.
- Laundry should be treated as contaminated, placed into an alginate bag and placed into a red laundry bag.
-
What Cleaning is required?
All equipment and the ambulance should have an in-between patient clean paying particular attention to touch points.
If a patient has been carried with a diagnosis of MRSA who is widely colonised and has a skin condition such as exfoliating dermatitis, is sputum positive and is actively coughing or has open, infected wounds then a hypochlorite solution should be used.
-
Do staff need any prophylaxis or follow up?
Staff do not routinely need to be followed up after caring for a patient with MRSA.




