Please click the frequently asked questions below for further information and IPC precautions required:
-
What is Mumps?
Mumps is a viral illness caused by a paramyxovirus, a member of the Rubulavirus family. The average incubation period for mumps is 16 to 18 days, with a range of 12 to 25 days.
Mumps complications include orchitis, oophoritis, mastitis, meningitis, encephalitis, pancreatitis, and hearing loss. Complications can occur in the absence of parotitis and occur less frequently in vaccinated patients. Some complications of mumps are known to occur more frequently among adults than children.
-
How does it spread?
The mumps virus replicates in the upper respiratory tract and is transmitted person to person through direct contact with saliva or respiratory droplets of a person infected with mumps. The risk of spreading the virus increases the longer and the closer the contact a person has with someone who has mumps.
The incubation period is around 17 days, with a range of 14 to 25 days. Individuals with mumps are
infectious from several days before the parotid swelling to several days after it appears
When a person is ill with mumps, they should avoid contact with others from the time of diagnosis until 5 days after the onset of swelling by staying home from work or school and staying in a separate room if possible.
-
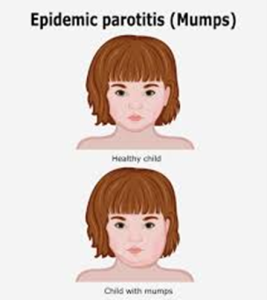
What are the symptoms of Mumps?
Mumps is best known for the puffy cheeks and tender, swollen jaw that it causes. This is a result of swollen salivary glands under the ears on one or both sides, often referred to as parotitis.
Other symptoms that might begin a few days before parotitis include:
- Fever
- Headache
- Muscle aches
- Tiredness
- Loss of appetite
Some people who get mumps have very mild symptoms (like a cold), or no symptoms at all and may not know they have the disease.

-
Why is this important?
If NIAS staff are aware that the patient has a suspected or confirmed case this should be communicated to the Control Room (Emergency or Non-emergency as appropriate) and the staff in the receiving unit when transferring the patient to ensure effective patient care and management.
-
IPC Precautions
- Droplet precautions should be used
- Hand Hygiene should be completed as per the 5 moments in line with usual practice.
- Eye protection should be risk assessed for any splash risks.
- A Fluid Resistant Surgical Mask should be worn.
- Gloves and Aprons should be worn.
- The patient should be transported via ambulance with no other patients present.
- Laundry should be treated as contaminated, placed into an alginate bag and placed into a red laundry bag.
-
What Cleaning is required?
All equipment and the ambulance should have an in-between patient clean paying particular attention to touch points.
-
Do staff need prophylaxis or follow up?
Immediate Action: Staff should inform their line manager and the IPC team at the earliest time able.
If staff have worn appropriate PPE with no breaches, then there is no follow up required.
If staff have evidence of mumps immunity including 2 doses of MMR vaccine no further input is usually required unless deemed high risk.
If no known immunity, they will be referred to Occupational Health and may be temporarily excluded from work. This will be risk assessed with input from OH, line management and the IPC team
All staff should remain vigilant for symptoms.
- Links to guidance




