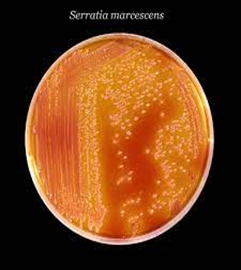
Serratia marcescens, a member of the Enterobacteriaceae family, is an important cause of invasive infections in neonatal intensive care units (NICUs), with significant associated morbidity and mortality.
Serratia marcescens causes infections such as pneumonia, urinary tract infection, wound infections and bacteraemia.
Risk factors for nosocomial infection of neonates include; low birth weight (<1500g), premature delivery, use of invasive devices, prolonged hospital stay and intensive care, prolonged use of antibiotics and maternal infection prior to delivery.
Death has also been reported in infants with severe conditions and/or congenital malformations, meningitis and septicaemia.