It is caused by organisms of the Mycobacterium tuberculosis complex, including M. tuberculosis, M. bovis and M. africanum. All three of these organisms are capable of causing TB in humans.
The risk of infection depends upon duration of exposure, the intensity of the exposure, and the immune status of the person exposed. The immune system clears the bacteria immediately in more than 80% of people exposed.
TB can present in a number of different ways. The most common are listed below:
Latent TB
In a small proportion of people who have been infected, the bacteria are walled off and remain dormant but viable. This is called latent TB. It is estimated that 5-10% of those with latent TB will develop active TB during their lifetime. Patients with latent TB are not considered infectious.
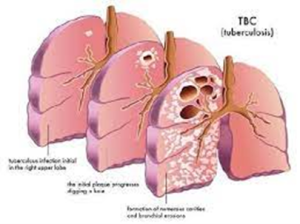
Active Pulmonary TB
The most infectious form of TB is pulmonary TB, particularly smear positive cases where TB bacilli can be seen on direct microscopic examination of the sputum. Left untreated, it is estimated that each person with active TB will infect on average between 10 and 15 people each year.
Closed TB
Non-pulmonary TB is less common than the pulmonary form and can involve any organ or tissue, most commonly bone, lymph nodes, central nervous system, skin and the genito-urinary tract. Patients with closed TB are not deemed to be infectious unless the infected area is disturbed, usually through an invasive procedure including surgery or open wound.
Multi Drug resistant TB (MDR-TB)
Sometimes drug-resistant TB occurs when bacteria become resistant to the drugs used to treat TB. This means that the drug can no longer kill the TB bacteria.
Drug-resistant TB is spread the same way that drug-susceptible TB is spread.
Extensively drug resistant tuberculosis (XDR-TB)
XDR-TB is a rare type of MDR-TB that is resistant to the most potent TB drugs. Patients are left with treatment options that are much less effective. XDR-TB is of particular concern for persons with HIV infection or other conditions that can weaken the immune system.