Please click the frequently asked questions below for further information and IPC precautions required:
-
What is VHF?
This is a High Consequence Infectious Disease (HCID) and the VHF plan should be triggered as soon as possible.
Viral haemorrhagic fevers (VHFs) are a diverse group of viral illnesses caused by five distinct RNA virus families. Some VHF agents cause only mild disease, but others can be severe and life-threatening. There are many VHF agents, a notable one being the Ebola virus. Others include Yellow fever virus, Dengue virus, Hantavrius and Crimean-Congo haemorrhagic fever virus etc.
VHF agents are found in areas of Africa, South America and Asia. Animals are the natural host, but humans are at risk of acquiring infection if they live in endemic areas and healthcare workers caring for those with VHF are at higher risk, especially if not equipped with the appropriate protective equipment.

-
How does it spread?
Transmission of VHFs varies depending on virus type. However, there are four main routes of transmission:
- Bites from infected ticks
- Bites from infected mosquitoes
- Direct contact with infected animals (especially rodents), waste products and carcasses
- Direct contact with infected persons, their body fluids and/or corpse
For those VHF agents that are transmitted via direct contact, many can continue to survive in body fluids outwith the infected host for several days. As such, transmission can occur when handling body fluids (e.g. urine, blood) or contaminated devices from an infected person or animal.
Some VHFs, such as Ebola, can remain contagious for several days after death and careful handling and disposal of the deceased is vital to reduce transmission. Of note, survivors of VHF have been found to carry the virus in their body fluids (e.g. urine, breast milk, semen) many months after symptoms abate.
The incubation Period varies, but is generally between 2 to 21 days.
-
What are the symptoms of VHF?
The symptoms and severity may depend on the causative organism. Symptoms may include:
- Aches and pains, such as severe headache and muscle and joint pain.
- Fever.
- Weakness and fatigue.
- Sore throat.
- Loss of appetite.
- Gastrointestinal symptoms including abdominal pain, diarrhoea, and vomiting.
- Unexplained haemorrhaging, bleeding or bruising.
-
Why is this important?
Due to the potential severe implications of this condition, an MDT and multi-agency approach will be crucial to the management of this patient.
VHFs are of particular public health importance because:
- They can spread readily within a hospital setting
- They have a high case-fatality rate
- They are difficult to recognise and detect rapidly
- There is no effective treatment.
If NIAS staff are aware that the patient has a suspected or confirmed case of VHF this should be communicated to the Control Room (Emergency or Non-emergency as appropriate) as this will trigger the VHF plan being activated.
This should also be communicated to the IPC team as soon as possible.
-
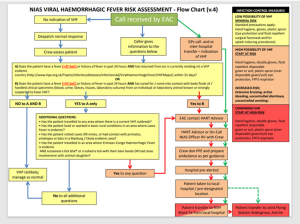
What will prompt a risk assessment for VHF?
For any patient who has had a fever [≥37.5°C] or history of fever in the previous 24 hours and a travel history or epidemiological exposure within 21 days will trigger a risk assessment by the IPC team and HART.
-
IPC Precautions
- This should be treated as a HCID.
- The HART team should be involved in risk assessment and transfer of all suspected and confirmed cases.
- As this is a HCID there are specific guidelines surrounding the use of PPE. Guidance should be sought for the appropriate method of donning and doffing of PPE.
- This is not an airborne disease however an FFP3 mask will be used.
- Ensure use of a buddy system for donning and doffing PPE.
- The NIAS guidance for VHF should be used and the IPC team contacted immediately for further advice.
-
What cleaning is required?
- All equipment and the ambulance should have a deep clean with a hypochlorite solution with a strength of 10,000 PPM (Same dilution as blood and body fluids).
- Appropriate PPE should be worn when decontaminating the vehicle and the equipment.
- Any single use equipment should be disposed of.
- Waste should be treated as Category 4 waste and disposed of in line with the trust waste.
-
NIAS VHF flowchart
-
Do staff need prophylaxis or follow up?
A list of staff will be recorded of all staff who have had interaction with the suspected/confirmed case.
All staff in contact with a case of VHF will be individually risk assessed by the multi-agency team.
- Links to guidance




