Please click the frequently asked questions below for further information and IPC precautions required:
-
What is Viral Meningitis?
Viral meningitis is the most common type of meningitis in adults and older children. It can be caused by many different viruses.
Non-polio enteroviruses are the most common cause of viral meningitis. Only a small number of people infected with enteroviruses will develop meningitis.
Other viruses that can cause meningitis are
- Mumps virus
- Herpesviruses, including Epstein-Barr virus, herpes simplex viruses, and varicella-zoster virus (which causes chickenpox and shingles)
- Measles virus
- Influenza virus
- Arboviruses, such as West Nile virus
- Lymphocytic choriomeningitis virus
To determine whether a person is suffering from viral or bacterial meningitis, doctors will have to perform a lumbar puncture.
Viral meningitis is almost never life-threatening.

-
How does it spread?
You can get viral meningitis by breathing in viral particles that have been sneezed or coughed into the air by another infected person. You can also become infected by touching surfaces contaminated with the virus, or through contact with faeces (for example, by changing nappies).
Close contacts of someone with viral meningitis can become infected with the virus that made that person sick. However, these close contacts are not likely to develop meningitis. Only a small number of people who get infected with the viruses that cause meningitis will develop viral meningitis.
-
What are the symptoms of Viral Meningitis?
Common symptoms in babies:
- Fever
- Irritability
- Poor eating
- Sleepiness or trouble waking up from sleep
- Lethargy (a lack of energy)
Common symptoms in children and adults:
- Fever
- Headache
- Stiff neck
- Photophobia (eyes being more sensitive to light)
- Sleepiness or trouble waking up from sleep
- Nausea
- Irritability
- Vomiting
- Lack of appetite
- Lethargy (a lack of energy)
Most people with mild viral meningitis usually get better on their own within 7 to 10 days.
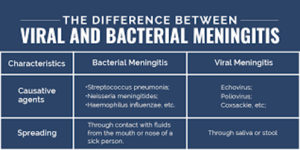
Initial symptoms of viral meningitis are similar to those for bacterial meningitis. However, bacterial meningitis is usually severe and can cause serious complications, such as brain damage, hearing loss, or learning disabilities. The pathogens (germs) that cause bacterial meningitis can also be associated with another serious illness, sepsis.
-
Why is this important?
If NIAS staff are aware that the patient has a suspected or confirmed case this should be communicated to the Control Room (Emergency or Non-emergency as appropriate) and the staff in the receiving unit when transferring the patient to ensure effective patient care and management.
-
IPC Precautions
- Hand Hygiene should be completed as per the 5 moments in line with usual practice.
- Eye protection should be risk assessed for any concern regarding a splash risk.
- Gloves and Aprons should be worn.
- The patient should be transported via ambulance with no other patients present.
- Laundry should be treated as contaminated, placed into an alginate bag and placed into a red laundry bag.
PPE may need to be increased depending on the causative virus! IPC advice should be sought.
-
What cleaning is required?
All equipment and the ambulance should have an in-between patient clean paying particular attention to touch points.
-
Do staff need prophylaxis or follow up?
Staff do not need to be routinely followed up or given prophylaxis. If the causative organism is known a risk assessment will be made with Occupational Health, the line manager and IPC team.




