Please click the frequently asked questions below for further information and IPC precautions required:
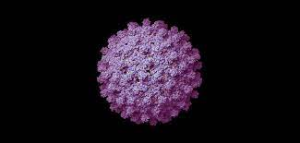
What is Hepatitis B (HBV)?
Hepatitis B is a serious liver infection caused by the hepatitis B virus (HBV). For most people, hepatitis B is short term, also called acute. Acute hepatitis B lasts less than six months, but can cause acute viral hepatitis (inflammation of the liver). For others, if the infection lasts more than six months, this is called chronic. Chronic hepatitis B raises the risk of liver failure, liver cancer and serious scarring of the liver called cirrhosis.
Most adults with hepatitis B recover fully, even if their symptoms are severe. Infants and children are more likely to develop a chronic, long-lasting hepatitis B virus infection.
How does it spread?
The virus passes from person to person through blood, semen or other body fluids. Common ways that HBV can spread are:
- Sexual contact. You may get hepatitis B if you have sex with someone who is infected and you don’t use a condom. The virus can pass to you if the person’s blood, saliva, semen or vaginal fluids enter your body
- Sharing of needles. HBV easily spreads through needles and syringes that are tainted with infected blood. Sharing equipment used to inject illicit drugs puts you at high risk of hepatitis B
- Accidental needlesticks. Hepatitis B is a concern for healthcare workers who come in contact with human blood
- Pregnant person to newborn. Pregnant people infected with HBV can pass the virus to their babies during childbirth
What are the main symptoms of Hepatitis B?
Symptoms of acute hepatitis B range from mild to serious. The symptoms usually start about 1 to 4 months after you’ve been infected with HBV. But you could notice them as early as two weeks after you’re infected. Some people with acute or chronic hepatitis B may not have any symptoms, especially young children.
Hepatitis B symptoms may include:
- Abdominal pain
- Dark urine
- Clay-coloured stool
- Fever
- Joint pain
- Loss of appetite
- Nausea and vomiting
- Extreme fatigue
- Jaundice
IPC Precautions
- Contact precautions should be used – this includes IPC practices in relation to blood/ body fluids and handling of sharps.
- Hand Hygiene should be completed as per the 5 moments in line with usual practice.
- Eye protection should always be risk assessed and used with any patient where there is a risk of splashes including spitting and productive coughing.
- Gloves and Aprons should be risk assessed.
- Laundry should be treated as per usual guidance unless contaminated with blood and body fluids. This should then be treated as contaminated and placed in an alginate bag and then into a red infected laundry bag.
What cleaning is required?
All equipment and the ambulance should have an in-between patient clean, paying particular attention to touch points.
Why is this information important?
If NIAS staff are aware that the patient has a suspected or confirmed case this should be communicated to the Control Room (Emergency or Non-emergency as appropriate) and the staff in the receiving unit when transferring the patient to ensure effective patient care and management.
Do staff need prophylaxis or follow up?
No follow up is required for staff unless there has been a needle stick injury or exposure to non-intact skin areas with blood or body fluids.
