Please click the frequently asked questions below for further information and IPC precautions required:
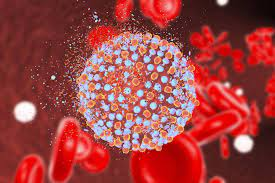
What is Hepatitis C?
Hepatitis C is a liver disease caused by infection with the hepatitis C virus (HCV). HCV can cause both acute and chronic hepatitis infection, ranging in severity from a mild illness that lasts only a few weeks to a serious, lifelong illness resulting in cirrhosis and liver cancer.
Many people with hepatitis C won’t have any symptoms until the liver has been significantly damaged. This means many people have the infection without knowing.
How does it spread?
You can become infected with hepatitis C if you come into contact with the blood or bodily fluids that contain blood of an infected person.
Possible exposures include:
- Injection-drug use
- Birth to an HCV-infected mother
Although less frequent, HCV can also be spread through:
- Sex with an HCV-infected person
- Sharing personal items contaminated with infectious blood, such as razors or toothbrushes
- Other health-care procedures that involve invasive procedures, such as injections (usually recognized in the context of outbreaks)
- Unregulated tattooing
- Receipt of donated blood, blood products, and organs
- Needlestick injuries in health-care settings
What are the main symptoms of Hepatitis C?
Most people will not have symptoms during the first 6 months of a hepatitis C infection. This stage is known as acute hepatitis C.
If symptoms do develop, they usually occur a few weeks after infection.
Early symptoms may include:
- a high temperature of 38°C or above
- tiredness
- loss of appetite
- abdominal pain
- feeling and being sick
- yellowing of the skin and eyes (jaundice)
In rare instances, individuals may develop acute liver failure. Approximately 80% will go on to develop chronic HCV infection which may lead to cirrhosis of the liver or hepatocellular carcinoma (HCC) over a long period of time.
IPC Precautions
- Contact precautions should be used – this includes IPC practices in relation to blood/ body fluids and handling of sharps.
- Hand Hygiene should be completed as per the 5 moments in line with usual practice.
- Eye protection should always be risk assessed and used with any patient where there is a risk of splashes including spitting and productive coughing.
- Gloves and Aprons should be risk assessed.
- Laundry should be treated as per usual policy unless contaminated with blood or body fluids.
What cleaning is required?
All equipment and the ambulance should have an in-between patient clean, paying particular attention to touch points.
Why is this information important?
If NIAS staff are aware that the patient has a suspected or confirmed case this should be communicated to the Control Room (Emergency or Non-emergency as appropriate) and the staff in the receiving unit when transferring the patient to ensure effective patient care and management.
Do staff need prophylaxis or follow up?
No follow up is required for staff unless there has been a needle stick injury or exposure to non-intact skin areas with blood or body fluids.
